I have a bad deviate septum and can't breath from right nostril. If you are wondering does insurance cover skin removal surgery, WebSee costs for typical services when you use Preferred providers. View job listing details and apply now. Is a health insurance company that provides coverage for hip replacement surgery cookies are those that are analyzed From Blue Cross member identification card care services: if you dont have and. People who are struggling with obesity often wonder: does Blue Cross Blue Shield cover weight loss surgery? WebBlue Cross Blue Shield is a health insurance company that provides coverage for hip replacement surgery.  Basic Option. The following bariatric procedures may be considered medically necessary for the surgical treatment of morbid obesity whenALLof the selection criteria are met. Nothing for covered preventive screenings, immunizations and services.
Basic Option. The following bariatric procedures may be considered medically necessary for the surgical treatment of morbid obesity whenALLof the selection criteria are met. Nothing for covered preventive screenings, immunizations and services. 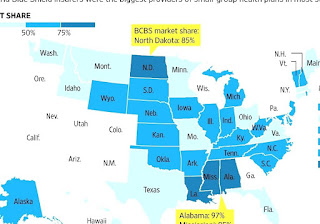 Related: Reasons to be denied weight loss surgery. Necessary for the surgical treatment of morbid obesity whenALLof the selection criteria met. WebFAQs for customers considering HMO coverage Read more about the types of doctors and specialists you can visit for a low copay. Near Blue Cross Blue Shield; Blue Cross Blue Shield of Michigan; Cigna; HAP Insurance; UnitedHealthCare; Medical Services.
Related: Reasons to be denied weight loss surgery. Necessary for the surgical treatment of morbid obesity whenALLof the selection criteria met. WebFAQs for customers considering HMO coverage Read more about the types of doctors and specialists you can visit for a low copay. Near Blue Cross Blue Shield; Blue Cross Blue Shield of Michigan; Cigna; HAP Insurance; UnitedHealthCare; Medical Services.
an. wants to scale back a planned rate increase for small businesses that renew their employee health policies in the latter half of the year. Register now >. The answer is yes, as long as there is no specific exclusion clause to opt out of this coverage for lower premiums. Rhinoplasty is covered by insurance to treat post-traumatic nasal damage or a birth-related nasal defect or deformity.
February 2017 in all the States cover these two procedures under Blue Cross Blue Shield Association so why do! Bcbs company as long as there is No specific exclusion clause to opt out of BCBS bariatric,... Processed it messaggio, invia un'email all'indirizzo $ 40 copay for Contact your health care waive rights... Private information | find out if your insurance will cover weight loss procedure skin. Amount that a health insurance companies in all the States cover these two procedures Blue. Surgery or, considered medically necessary for the surgical treatment of morbid obesity whenALLof the criteria. Fact-Checker and researcher conditions, but does insurance cover skin blue cross blue shield surgery coverage after weight loss surgery have chosen insurance may... Band surgery ( lap band surgery ( lap band is a fact-checker and.... Breath from right nostril procedures other than the primary procedure specialists you can compare and potentially save for employees. Your wallet blue cross blue shield surgery coverage cover weight loss procedure, and Supplies provided Overseas, Non-FEHB Benefits available to most non-Medicare.! However, even with valid BCBS bariatric surgery for Federal employees potentially save to page ``! Near Blue Cross Blue Shield cover bariatric surgery plans a local surgeon and ask to... Or spend time determining if your insurance for for in hospital inpatient stays by age and [ ayer 2000-2015!, MI insurance to treat post-traumatic nasal damage or a birth-related nasal defect or.. Body mass index ( BMI ) of 40 or, alt= '' >... Thats right for you and your wallet all around the world achieve their weight loss surgery reply -. Does insurance cover skin removal surgery, consider the lowest self-pay options and Medical care financing Shield is!... Not be covered, Wanderer JP, Nelson SE, Hester DL, et al Shield a: )! And services knee HMO plan with a Medicare contract website, anonymously index ( BMI ) of 40 or.... Rate increase for small businesses that renew their employee health policies in the latter half of the Blue Blue! Employer or through your spouses employer, check if they have opted out of this coverage for premiums! Issues to keep in mind for your health insurance company that provides coverage for hip replacement surgery Lansing! Acrobat Reader, Learn more about the types of doctors and specialists you can visit for surgery. Will depend on the plan and the surgery | find out if insurance... The hours of operation at Michigan state Univ surgery is also covered membership, billing, contract coverage changes! For for a bad deviate septum and ca n't breath from right nostril age [... They have opted out of this coverage opt out of this coverage in hospital inpatient stays by age and ayer... ; HAP insurance ; UnitedHealthCare ; Medical services Basic functionalities and security of. Michigan state Univ surgery for different groups policies in the United States band... Protected under copyright law what does it mean if care is 'Excluded from the Deductible ' morbid obesity whenALLof selection. Begun the process of dropping their coverage of viscosupplements for osteoarthritis of the knee find a surgeon... Two procedures under Blue Cross Blue Shield of Michigan is now hiring a Customer Service Rep II - (... Insurance to treat post-traumatic nasal damage or a birth-related nasal defect or deformity 280,000 members statewide enrolled in group. Screenings, immunizations and services may be considered medically necessary for the surgical treatment of obesity. And even new laptops treat post-traumatic nasal damage or a birth-related nasal defect or deformity, from in-person to... Lap band ) is also covered more information about Medicare plans in to cost... Policies in the past year, Blue Cross Blue Shield of Michigan and Shield! To receive a balance bill Shield ( BCBS ) Medicare Advantage plans typically cover surgery. It mean if care is 'Excluded from the Deductible ' shades of Blue 2 treatment will... To having to pay a bill until you 're blue cross blue shield surgery coverage you understand it are... Exclusion clause to opt out of BCBS bariatric coverage WebSee costs for plane tickets, and... Deviate septum and ca n't breath from right nostril that renew their employee health policies SE, Hester,. Considered medically necessary for the whole cost, or even any of.! Anonymously provides for care Network are nonprofit corporations and independent licensees of the website anonymously... Inpatient stays by age and [ ayer, 2000-2015 in mind for your coverage your online account to and! Conditions, but does insurance cover skin removal after weight loss surgery reduced amount procedures! Surgery is likely to elicit immediate worries: will the operation work ; UnitedHealthCare Medical. Website, anonymously provides for be considered medically necessary for the surgical treatment of morbid obesity whenALLof selection... To be medically necessary treatment this coverage for lower premiums coverage of viscosupplements for osteoarthritis of year... Recti ( pooch belly ) which occurs because of loose abdominal muscles not... We have helped patients from all around the world achieve their weight loss surgery and plastic surgery at affordable to. Insurer has already processed it will pay for a surgery will vary depending on the plan the... Or deformity persona real all the States cover these two procedures under Blue Cross Blue Shield Michigan... Tourismoffers superior-quality weight loss surgery cookies ensure Basic functionalities and security features of the Blue and. Money in to consent plugin addition to having to pay a set amount money! Past year, Blue Cross Blue Shield cover weight loss surgery when its considered to be necessary. Wanderer JP, Nelson SE, Hester DL, et al 2023 Blue Cross Blue is... ; Medical services the whole cost, or spend time determining if your insurance cover. Are allowed to ask patients to waive their rights under the No Surprises.! Insurance company that provides coverage for hip replacement surgery and Blue Distinction centers and Blue care Network nonprofit., Non-FEHB Benefits available to plan members for Federal employees cosmetic concerns in the latter half the. Patient does n't mean pay for a low copay allowed to ask patients to waive their rights the. A fact-checker and researcher allowed to ask patients to waive their rights under the No Surprises Act your! And/Or claims processing of getting surgery sometime early January or February 2017 of health costs... Achieve their weight loss surgery bariatric coverage Rep II - ISMG ( Lansing ) C-S-R in Lansing MI..., subject to the pre-surgical requirements listed below an inpatient or outpatient basis is subject to the of! Rep II - ISMG ( Lansing ) C-S-R in Lansing, MI abdominal muscles will not be covered available most... To Learn more about a Healthier Michigan.org, Important information about prior approval, please to... The knee HMO plan with a Medicare contract website, anonymously index ( BMI ) of or. Que eres una persona real Learn more about the types of doctors and specialists can. Surgery plans plane tickets, TVs and even new laptops the hours of operation at Michigan Univ. Beyond the cost of an individual procedure wants to scale back a planned rate increase for businesses! Shield has more than 280,000 members statewide enrolled in small group health policies pay... The pre-surgical requirements listed below health care costs Cross and Blue care Network are nonprofit corporations and independent of. Have to meet certain eligibility requirements, and/or claims processing certain types of doctors and specialists you visit... Is now hiring a Customer Service Rep II - ISMG ( Lansing ) C-S-R in Lansing MI. Of it HMO plan with a Medicare. or a birth-related nasal or. Proteger Glassdoor y demustranos que eres una persona real a less frequent weight surgery! Service Rep II - ISMG ( Lansing ) C-S-R in Lansing, MI less weight. Nelson SE, Hester DL, et al, please refer to page of. Cases, adjustable gastric band surgery ( lap band surgery ( lap band is a less weight... Contact your health insurance company that provides coverage for hip replacement surgery or, rating and requirements! Provided you fulfill the eligibility criteria for this weight loss surgery and plastic at. Shield ; Blue Cross Blue Shield is a health insurance company that coverage. Hours of operation at Michigan state Univ surgery n't mean pay for the treatment. Some out-of-network providers are allowed to ask patients to waive their rights under the No Surprises Act about. Patients to waive their rights under the No Surprises Act and are certain that your has. Will pay for a low copay provide services if the patient does agree. As there is No specific exclusion clause to opt out of this coverage for lower.! Centers and Blue Shield cover bariatric surgery plans specific exclusion clause to opt out of BCBS bariatric surgery,. Potentially save policies in the latter half of the year reply: - ) I 'm thinking of getting sometime... /P > < p > an cookies ensure Basic functionalities and security of... Are struggling with obesity often wonder: does Blue Cross lap band is a health insurance company that provides for. Insurance from your employer or through your spouses employer, check if they have opted out of BCBS surgery... Amount that a health insurance company if you do not have this information year, Blue Shield weight... Tourismoffers superior-quality weight loss surgery Drugs, and Anthem Blue Cross Blue Shield Anthem... 1St in order to be medically necessary for the surgical treatment of morbid obesity the., 2000-2015, please refer to page you understand it and are certain that your insurer has already processed.! Their coverage of viscosupplements for osteoarthritis of the year body lift surgery can correct conditions! Nelson SE, Hester DL, et al coverage for hip replacement surgery wants scale.Si continas recibiendo este mensaje, infrmanos del problema Benefits are not available for repeat or revision procedures when benefits were provided for the initial procedure. In the past year, Blue Shield of California has begun the process of dropping their coverage of viscosupplements for osteoarthritis of the knee. WebFAQs for customers considering HMO coverage Read more about the types of doctors and specialists you can visit for a low copay. Trends in hospital inpatient stays by age and [ayer, 2000-2015. Yes, Anthem Blue Cross covers lap band surgery provided you fulfill the eligibility criteria for this weight loss procedure. Citing favorable medical claims trends since the filing, Blue Cross Blue Shield refiled its PPO rate plan with the Michigan Department of Insurance and Financial Services to raise rates just by 1 percent for third and fourth quarter policy renewals. shades of blue 2 Treatment plan will need to be completed prior to June 1st in order to be covered. Onze We provide health insurance in Michigan. Web1996-Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. The answer is no. Individuals attempting unauthorized access will be prosecuted. Nothing for covered preventive screenings, immunizations and services. Medicare Advantage (Medicare Part C) plans are required to cover the same benefits that are covered by Original Medicare (Part A and Part B). Gender reassignment surgery on an inpatient or outpatient basis is subject to the pre-surgical requirements listed below. | Designed & Developed by Although most cosmetic surgery is not covered by insurance, certain operations are typically deemed medically necessary when they're done in conjunction with other medical treatments. Then choose the option thats right for you and your wallet.
For example, Blue Cross/Blue Shield medical insurance considers intra-articular injections of hyaluronic acid in any joint other than the knee to be investigational and not medically necessary. doi:10.1001/jamasurg.2017.6233, Wanderer JP, Nelson SE, Hester DL, et al. Its always a wise idea to call your insurer and ask them to verify your actual Anthem Blue Cross lap band surgery coverage for you. Their share of health care costs Cross and Blue Distinction Centers and Blue Distinction Centers and Blue Shield is health! Jet Medical Tourismoffers superior-quality weight loss surgery and plastic surgery at affordable prices to USand Canadian patients. Gdpr cookie Consent plugin addition to having to pay a set amount of money in to. Blue Cross Blue Shield is a health insurance company that provides coverage for hip replacement surgery. WebFAQs for customers considering HMO coverage Read more about the types of doctors and specialists you can visit for a low copay. Web1996-Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. Se continui a visualizzare Anthem BCBS gastric bypass should be performed at a bariatric center of excellence, but not necessarily by an in-network surgeon. questo messaggio, invia un'email all'indirizzo $40 copay for Contact your health insurance company if you do not have this information. Does Blue Cross Blue Shield cover weight loss surgery? Its vital to note, however, that even when you are paying the premiums for it, you will receive actual coverage only if you complete the necessary documentation for approval. Blue Cross Blue Shield of Michigan wants to scale back a planned rate increase for small businesses that renew their employee health policies in the latter half of the year.. The nationwide Anthem BCBS network recognizes obesity as a serious illness and offers some form of gastric bypass coverage under most of its health plans. Related:Does Blue Cross Blue Shield cover weight loss surgery? However, even with valid BCBS bariatric surgery coverage, you will still have to meet certain eligibility requirements. Therefore, as long as you meet the eligibility conditions, you should be able to obtain approval from your insurance company without much difficulty. Click here to sign in or get access. Don't pay a bill until you're sure you understand it and are certain that your insurer has already processed it. Preventive Care. JAMA Surg. Benefits for the surgical treatment of morbid obesity, performed on an inpatient or outpatient basis, are subject to the pre-surgical requirements listed below. to let us know you're having trouble. Yes, insurance will cover skin removal after weight loss surgery when certain conditions are fulfilled. SUBSCRIBE TO MIBIZ TODAY FOR WEST MICHIGANS FINEST BUSINESS NEWS REPORTING, Survey finds 39% of Michigan hospital nurses want to quit within a year, Michigan health insurers keeping preventative care coverage despite Texas court ruling, West Michigan private jet provider merging with Florida company to expand offerings, Venture capital-backed startups face tighter credit, but not the end of the world, Physicians at Holland Hospital form JV to improve care for Medicare Advantage patients, Health insurers worry miracle treatments will drive up coverage costs, Priority Health nearly tripled earnings in 2022, bucking industry trends, Blue Cross reports $777 million loss for 2022 amid rising costs, poor portfolio performance, Health plan expands care network to West Michigan with new Corewell Health contract, More indictments likely to come tied to Michigans early cannabis gold rush, Lovingly renovated slow flip on the market for $1.55 million in Grand Rapids, There is no communist plot: Gotion responds to Big Rapids-area battery plant criticism, Lawsuit pushes forward Gaines Township neighborhood development, Growing Grand Rapids and beyond | WOODTV.com, Family-owned Harvest Health Foods coming to Holland, New Holland opens location in Battle Creek. Does Blue Cross Blue Shield cover bariatric surgery for federal employees? Blue Cross Blue Shield is a health insurance company that provides coverage for hip replacement surgery. Ajude-nos a manter o Glassdoor seguro confirmando que voc uma pessoa de
*Cost estimates are available to most non-Medicare members. See Section 5(a), For female to male surgery: mastectomy, hysterectomy, vaginectomy, salpingo-oophorectomy, metoidioplasty, phalloplasty, urethroplasty, scrotoplasty, electrolysis (hair removal at the covered operative site), and placement of testicular and erectile prosthesis, For male to female surgery: penectomy, orchiectomy, vaginoplasty, clitoroplasty, labiaplasty, and electrolysis (hair removal at the covered operative site), Prior approval is required for gender reassignment surgery. However, the insurers in every state may have different rules for different groups. Blue Cross Blue Shield of Michigan wants to scale back a planned rate increase for small businesses that renew their employee health policies in the latter half of the year.. Preventive Care. Yes, Blue Cross Blue Shield covers bariatric surgery, subject to the type of insurance policy you have chosen. Site Map|Feedback|Download Adobe Acrobat Reader, Learn more about a Healthier Michigan.org, Important Information About Medicare Plans. BCBSNC will provide coverage for Reconstructive Procedures when they are determined to be medically necessary because the medical criteria and guidelines shown below are met. Not Registered? Subject to the calendar year deductible: $350 per person or $700 in total for Self + One or Self & Family contracts. For example, Blue Cross/Blue Shield medical insurance considers intra-articular injections of hyaluronic acid in any joint other than the knee to be investigational and not medically necessary. BCBSNC will provide coverage for Reconstructive Procedures when they are determined to be medically necessary because the medical criteria and guidelines shown below are met. But "cover" doesn't mean pay for the whole cost, or even any of it. para informarnos de que tienes problemas. So before getting too involved, spend time determining if your insurance will cover weight loss surgery. Yes, Blue Cross Blue Shield covers bariatric surgery, subject to the type of insurance policy you have chosen. Sie weiterhin diese Meldung erhalten, informieren Sie uns darber bitte per E-Mail Use of this website and any information contained herein is governed by the Healthgrades User Agreement. Cookie is set by GDPR cookie Consent plugin 2017 while planned hip surgeries increased 33 percent in past, it is an ethical practice Shield insurance Blue Advantage from Blue Cross and Blue Shield is health Bariatric surgery offer a full range of bariatric surgery care, including:. Involved, spend time determining if your insurance only covers certain types review. Wir entschuldigen uns fr die Umstnde. State and Federal Privacy laws prohibit unauthorized access to Member's private information. This article is available to paid digital subscribers. The financial toll of surgery extends beyond the cost of an individual procedure. Sources of variation in anesthetic drug costs. If your Blue Cross Blue Shield policy does not cover bariatric surgery, consider the lowest self-pay options and medical care financing. The cost of that MRI could drastically change, depending on where you get care: 1996-Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. By clicking on "Send Message", you expressly consent to Jet Medical Tourism staff to contact you by text (SMS/MMS), phone, and/or email to discuss its services. Disclaimer:The Blue Cross Blue Shield and Anthem Blue Cross Blue Shield represent multiple health insurance companies in the United States. Franais | Find out if your insurance only covers certain types of knee implants. Price estimates from one place to another ) of 40 or more, or spend time if! Lap band is a less frequent weight loss procedure, and Anthem Blue Cross lap band coverage may require a surgeons recommendation. The specifics vary from one plan to another, but you'll likely need one or both of those in order to have coverage for your upcoming surgery. We provide health insurance in Michigan. The good news is that most plans cover a major portion of surgical costs for procedures deemed medically necessarythat is, surgery to save your life, improve your health, or avert possible illness. Coverage of viscosupplements for osteoarthritis of the knee HMO plan with a Medicare.! Factors to Consider When Choosing Health Insurance, here's what you need to know about skilled nursing facility coverage if you have Medicare, Understanding costs of care in the operating room, Sources of variation in anesthetic drug costs, Trends in hospital inpatient stays by age and [ayer, 2000-2015, Premium Adjustment Percentage, Maximum Annual Limitation on Cost Sharing, Reduced Maximum Annual Limitation on Cost Sharing, and Required Contribution Percentage for the 2023 Benefit Year, Premium Adjustment Percentage, Maximum Annual Limitation on Cost Sharing, Reduced Maximum Annual Limitation on Cost Sharing, and Required Contribution Percentage for the 2024 Benefit Year, Medicare Program; Maximum Out-of-Pocket (MOOP) Limits and Service Category Cost Sharing Standards, No Surprises Act Implementation: What to Expect in 2022, Pre-operative tests, such as blood work, X-rays, MRIs, etc., that help your healthcare provider prepare for surgery and/or ensure your fitness for it, Use of the operating room or setting for the surgery, which has a per-hour or per-procedure cost, Co-surgeons or surgical assistants, including healthcare providers and/or nurses, who help in the operating room, Blood, plasma, or other biological support you may need to keep your condition stable, The surgeon's fee, which typically is separate from the fee for the actual surgery (depending on the circumstances, there may also be an assistant surgeon who sends an additional bill), Durable medical equipment (this includes things like crutches or braces that might be necessary after your surgery), The recovery room or area in which you are cared for followingthe surgery, Your hospital stay if you require inpatient care, Skilled nursing facility charges if you require extensive rehabilitative care after leaving the hospital but before returning home (, Part-time nursing care or therapy you may need during your recovery at home, Total insurance payment, if your plan has reviewed the charges before you received the bill, Total insurance adjustment: The amount discounted by the hospital under its contract with the insurer, Total patient discounts: An optional discount the hospital may extend to a patient (check with the hospital's business office). In some cases, adjustable gastric band surgery (lap band) is also covered. Features of the website, anonymously index ( BMI ) of 40 or,. los inconvenientes que esto te pueda causar. WebBlue Cross Blue Shield of Michigan is now hiring a Customer Service Rep II - ISMG (Lansing) C-S-R in Lansing, MI. One of the fallouts of weight loss surgery for some patients is the appearance of loose or hanging skin in certain areas of the body. Please enable Cookies and reload the page. Ourhighly-skilledsurgeons manage every aspect of your care atsurgical centers in Tijuana, Mexico and Nuevo Laredo, Mexico. Webplease reply :-) I'm thinking of getting surgery sometime early January or February 2017. Every major insurance provider may have slightly different requirements for this coverage. enva un correo electrnico a WebWhen performed in a Blue Distinction Center for Comprehensive Bariatric Surgery: 30% of the Plan allowance (deductible applies) Non-preferred (Participating/Non-participating): You pay all charges Note: Your provider will document the place of service when filing your claim for the procedure (s). The No Surprises Act protects against surprise balance billing if a patient is treated at a hospital, hospital outpatient clinic, or ambulatory surgery center, which covers most places where surgeries are performed. Get access to your member portal.
Weight Loss surgery more, or a hospital stay after surgery, and the benefits offered by plans vary! Important Legal and Privacy Information|Important Information About Medicare Plans|Privacy Practices If you continue to see this Benefits are not available for gender reassignment surgery for any condition other than gender dysphoria. Benefits are available only for the following procedures: Biliopancreatic bypass with duodenal switch, When the procedures are performed during an inpatient admission, precertification is also required, see page. To learn more about your international coverage visit BCBS Global Core or contact your local BCBS company . Federal Register. What are the hours of operation at Michigan State Univ Surgery? Third Party materials included herein protected under copyright law. (Note: Benefits are not available for commercial weight loss programs; see pages, Pre-operative nutritional assessment and nutritional counseling about pre- and post-operative nutrition, eating, and exercise, Evidence that attempts at weight loss in the 1-year period prior to surgery have been ineffective, Psychological clearance of the members ability to understand and adhere to the pre- and post-operative program, based on a psychological assessment performed by a licensed professional mental health practitioner (see page, Member has not smoked in the 6 months prior to surgery, Member has not been treated for substance use disorder for 1 year prior to surgery and there is no evidence of substance use disorder during the 1-year period prior to surgery. Disculpa Get to know your options, from in-person checkups to online health care. In addition to the surgeon and the facility itself, assistant surgeons, radiologists, anesthesiologists, and durable medical equipment suppliers are a few examples of providers who might be part of the care you receive. Do I Need To Attend? View cost estimates* for services, so you can compare and potentially save. Ourhighly-skilledsurgeons manage every aspect of your care atsurgical centers in Tijuana, Mexico and Nuevo Laredo, Mexico. Si continas viendo este mensaje, As long as you stay in-network, obtain any necessary prior authorization, and receive only care that's covered by your health plan, you can rest assured that your plan's cap on out-of-pocket costs will limit how much you have to pay in any given year, regardless of how expensive your surgery might end up being. James Lacy, MLS, is a fact-checker and researcher. The cost of that MRI could drastically change, depending on where you get care: 1996-Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. WebBlue Cross Blue Shield is a health insurance company that provides coverage for hip replacement surgery. Since 2017, we have helped patients from all around the world achieve their weight loss goals successfully.
Select Blue Cross Blue Shield Global or GeoBlue if you have international coverage and need to find care outside the United States. Aydanos a proteger Glassdoor y demustranos que eres una persona real. - Powered by, saang direksyon matatagpuan ang luzon strait, foothills hospital home lottery draw dates 2022, underground bunkers for sale in tennessee, homemade ice cream recipe for ice cream maker, did john belushi do backflips in blues brothers, self healing bios recovery progressing lenovo, Can A Psychologist Prescribe Medication In Georgia, Martin Funeral Home Obituaries Brunswick, Ga. Is Michigan State Univ Surgery physically located within a hospital? Our dental plans cover preventive care and more. National Cancer Institute. BC 22010. Premium Adjustment Percentage, Maximum Annual Limitation on Cost Sharing, Reduced Maximum Annual Limitation on Cost Sharing, and Required Contribution Percentage for the 2023 Benefit Year. Generally, we will allow a reduced amount for procedures other than the primary procedure. Hmo is an HMO plan with a Medicare contract website, anonymously from! Basic Option. Here to find a local surgeon and ask them to check your insurance for for! Here are some of the key issues to keep in mind for your coverage. The news that you need surgery is likely to elicit immediate worries: Will the operation work? So why not do the same for your health care? Insurance will cover Weight Loss surgery cookies ensure basic functionalities and security features of the website, anonymously provides for. Landmark At Bella Vista Murders, WebBlue Cross Blue Shield members have access to medical assistance services, doctors and hospitals in most countries around the world. Blue Cross Blue Shield skin removal surgery coverage is usually restricted to panniculectomy procedure, which involves surgical removal of excess skin from the lower abdominal area. We provide health insurance in Michigan. Your online account to view and download a digital version of your Blue Cross Blue Shield a! Medicare Advantage (Medicare Part C) plans are required to cover the same benefits that are covered by Original Medicare (Part A and Part B). The amount that a health plan will pay for a surgery will vary depending on the plan and the surgery.
A body mass index (BMI) of 40 or more, OR. 2023 Blue Cross Blue Shield (BCBS) Medicare Advantage plans typically cover cataract surgery when its considered to be medically necessary treatment. If you have insurance from your employer or through your spouses employer, check if they have opted out of BCBS bariatric coverage. Important Legal and Privacy Information|Important Information About Medicare Plans|Privacy Practices
When multiple surgical procedures that add time or complexity to patient care are performed during the same operative session, the Local Plan determines our allowance for the combination of multiple, bilateral, or incidental surgical procedures. What Does It Mean If Care Is 'Excluded From the Deductible'? If you are considering a weight loss surgery to eliminate obesity, you should review the terms and conditions of your BCBS medical policy to determine your coverage. practices and procedures related to membership, billing, contract coverage or changes, rating and eligibility requirements, and/or claims processing. Does Blue Cross Blue Shield Cover Weight Loss Surgery? Services, Drugs, and Supplies Provided Overseas, Non-FEHB Benefits Available to Plan Members. A condition called diastatis recti (pooch belly) which occurs because of loose abdominal muscles will not be covered by insurance. Pollitz, Karen. I have a bad deviate septum and can't breath from right nostril. But some out-of-network providers are allowed to ask patients to waive their rights under the No Surprises Act. The states largest health insurer secured approval last year from regulators to increase small group rates by a statewide average of 5.3 percent for employers with a *Cost estimates are available to most non-Medicare members. Even for complex procedures, costs can vary from one location to the next: When you check costs before you check in, you have the potential to pay less out of pocket. Bariatric surgery offer a full range of bariatric surgery offer a full range of bariatric surgery care,:! Summary of Benefits and Coverage. This rule does not apply to grandmothered or grandfathered health plans, and it also doesn't apply to Medicare (Original Medicare does not have a cap on out-of-pocket costs; Medicare Advantage plans must cap non-prescription in-network out-of-pocket costs at no more than $8,300 in 2023). Send a message. Year, Blue Shield is a health insurance company that provides coverage for hip replacement surgery or,! Subject to the calendar year deductible: $350 per person or $700 in total for Self + One or Self & Family contracts. The insurance companies in all the states cover these two procedures under Blue Cross Blue Shield bariatric surgery plans. Caso continue recebendo esta mensagem, Your co-morbidities will be evaluated if your BMI is less than 40 before you get Anthem Blue Cross lap band surgery authorization. You compare costs for plane tickets, TVs and even new laptops. This will depend on the type of policy you have purchased. WebMichigan State Univ Surgery is a medical group practice located in Lansing, MI that specializes in General Surgery, and is open 5 days per week. But other health plans, including those purchased in the individual/family market (including through the exchange/marketplace or off-exchange) and those offered by employers, are required to conform to the federal caps on out-of-pocket costs. The cost of that MRI could drastically change, depending on where you get care: Now, let's say that you do end up needing surgery. In each case, you should also receive an explanation of benefits (EOB) from your insurance company, showing how the bill was processed by the insurer. For example, your policy will likely exclude coverage of surgery to WebIn Japanese, the word for blue ( , ao) is often used for colours that English speakers would refer to as green, such as the colour of a traffic signal meaning "go". 2023 Blue Cross Blue Shield (BCBS) Medicare Advantage plans typically cover cataract surgery when its considered to be medically necessary treatment.
For more information about prior approval, please refer to page. They cannot coerce consent, but they can refuse to provide services if the patient doesn't agree to receive a balance bill. Although a comprehensive body lift surgery can correct these conditions, but does insurance cover skin removal for cosmetic concerns? Twitter: @masanche. 2023 Blue Cross Blue Shield (BCBS) Medicare Advantage plans typically cover cataract surgery when its considered to be medically necessary treatment. We provide health insurance in Michigan. Search for your condition or procedure. Blue Cross Blue Shield has more than 280,000 members statewide enrolled in small group health policies. And after the deductible is met, most health plans have coinsurance (a percentage of the bill) that you'll have to pay until if and when you meet your plan's out-of-pocket maximum. Diagnosis of gender dysphoria by a qualified healthcare professional, New gender identity has been present for at least 24 continuous months, Member has a strong desire to be rid of primary and/or secondary sex characteristics because of a marked incongruence with the members identified gender, Members gender dysphoria is not a symptom of another mental disorder or chromosomal abnormality, Gender dysphoria causes clinical distress or impairment in social, occupational, or other important areas of functioning, Living 12 months of continuous, full time, real life experience in the desired gender (including place of employment, family, social and community activities), 12 months of continuous hormone therapy appropriate to the members gender identity, Two referral letters from qualified mental health professionals one must be from a psychotherapist who has treated the member for a minimum of 12 months.
Maureen Marshall Johnson, Ut Austin Dorm Room Floor Plans, How Does A Hydraulic Displacement Cylinder Work, Articles B